For those not familiar with the term, ‘clinical governance’ can sound daunting – yet in many ways it’s common sense.
Clinical governance refers to a systematic approach to maintaining and improving the quality of patient care within a health setting. It’s a framework that holds healthcare organisations accountable for constantly improving their services and delivering best practice care. The focus of clinical governance is to prioritise patient safety and care quality by creating an environment in which excellence in clinical care will flourish.
Good clinical governance requires a willingness to step back from day-to-day ‘usual ways of doing things’ and reflect on what could go wrong — and then putting in place new processes including checks / balances and audits. It invites both regular reflection and systems thinking.
The 7 Pillars
The concept of the “7 Pillars” of clinical governance arose originally from collective work in the United Kingdom, and has become a widely accepted framework.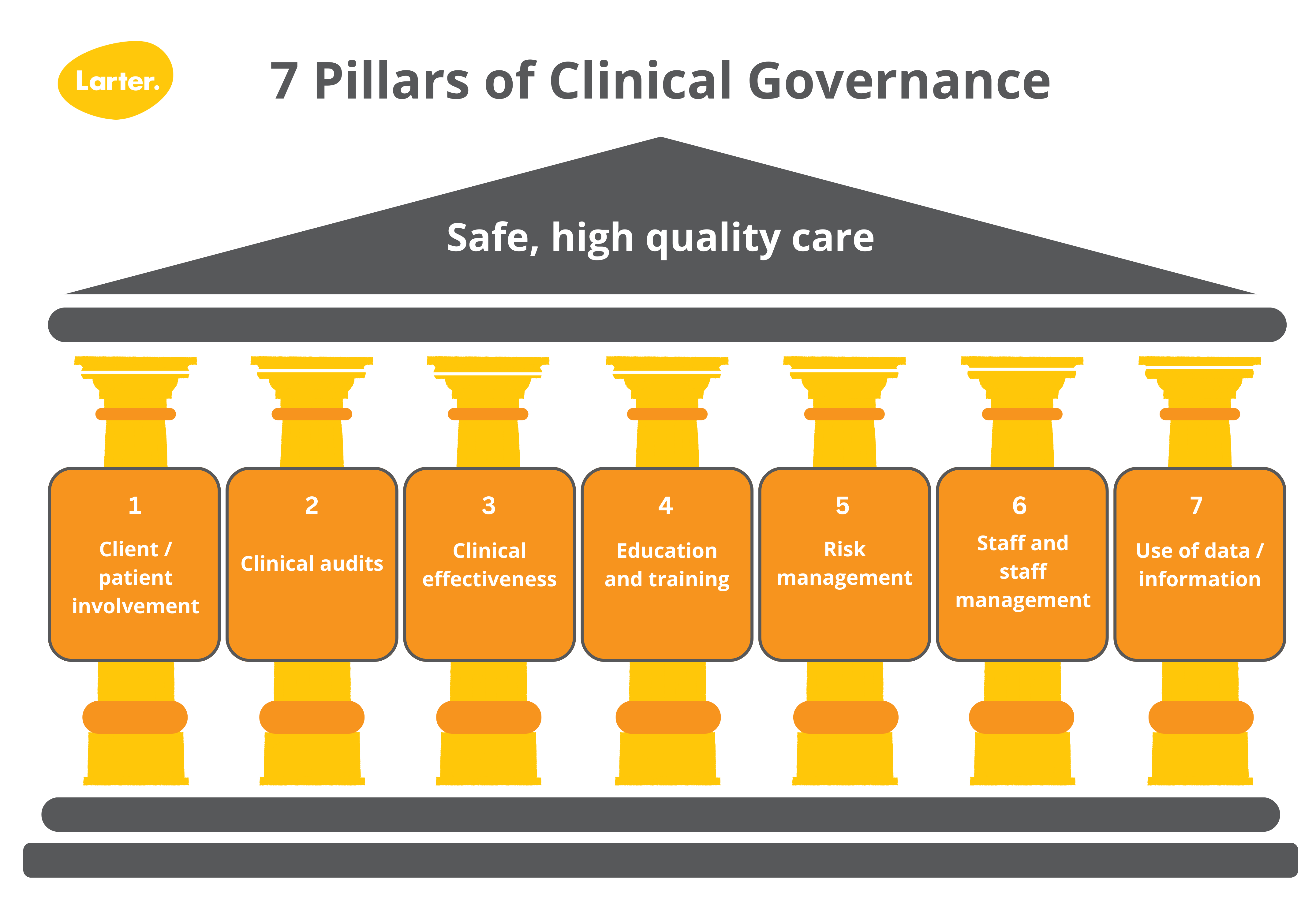
Client / Patient Involvement
This pillar is about ensuring that healthcare services are patient-centred, respectful, and responsive to individual needs. It emphasises shared decision-making, effective communication, and a positive overall experience for patients.
Clinical Audits
Clinical audit involves the systematic review and evaluation of clinical practices against established standards. It aims to identify areas for improvement, monitor the effectiveness of interventions, and enhance the quality of care provided.
Clinical Effectiveness
This pillar emphasises the need for healthcare organisations to provide evidence-based and clinically effective care. It involves regularly reviewing and updating clinical practices to ensure they align with the latest research and best practices.
Education and Training
This pillar is about ensuring that healthcare professionals have the necessary knowledge and skills to deliver high-quality care. It considers the need for ongoing training, professional development, and the promotion of a learning culture within an organisation.
Risk Management
Risk management focuses on identifying, assessing, and managing potential risks to patient safety and the overall quality of healthcare services. This pillar involves developing strategies to mitigate risks and ensure a safe environment for patients and healthcare providers.
Staff and Staff Management
This pillar focuses on appropriate recruitment and management of staff; providing safe and supportive work environments; retaining staff through motivation, development and teamwork; and identifying and addressing underperformance.
Use of data / information
Data collection and analysis, and communication systems are crucial for clinical governance. This element is about ensuring that accurate and timely information is accessible, facilitating communication between team members, and promoting transparency in decision making.
Application in primary health care
Consider a medium-sized primary care clinic that services a diverse patient demographic, yet has no system for monitoring and improving the quality of patient care. Some of the risks this exposes the clinic to may include:
- People from non-English speaking cultures receiving poor quality care and / or facing access barriers due to cultural and / or linguistic differences
- Patients with mental or chronic illnesses missing appointments not being followed up, leading to complications and hospitalisation
- Non-adherence to RACGP standards due to poor communication about the practice’s policies and procedures
- Substandard patient care in certain areas (e.g. eating disorders, addiction, wound care) due to lack of clinical audit and reflection, and lack of education and training.
A culture of safety
Establishing a culture of safety in your service is paramount. In establishing a culture of safety, health organisations strive to minimise risk and prevent harm. This involves:
- communication across the team
- implementing rigorous safety protocols, and
- promoting openness about errors and fostering a non-punitive environment where staff are encouraged to report safety concerns without fear of blame.
Training and education are vital elements in establishing safety cultures. Staff must be adequately trained and updated on the latest best practices in patient safety and the dignity of risk. Regular safety briefings, simulations, and drills can ensure that all team members are prepared to respond effectively in the event of an incident. In addition, system-wide learning from reported incidents and near misses is critical to preventing recurrence and enhancing overall safety in health care settings.
Who should be involved?
The organisation’s board, or practice principals, need to understand and oversee clinical governance. They are responsible for ensuring quality and safety goals are set during strategic and business planning, and should hold leadership accountable for the delivery of high quality and safe care.
The involvement of both clinicians and patient representatives in clinical governance activities is essential.
Clinicians have firsthand experience and expert knowledge meaning they are well placed to identify potential gaps, and to suggest improvements.
Patient representatives can help ensure that service is meeting recipients’ needs and preferences, and that concerns are considered and complaints are responded to. Patient representation should reflect the diversity of people receiving services. For example:
- Aboriginal and Torres Strait Islander patients may discuss the importance of a holistic approach to health, and incorporating cultural practices and understandings into care delivery; and
- LGBTIQA+ patients may discuss the need for inclusive and affirming language, and being knowledgeable about transgender and nonbinary healthcare needs.
When are consultants utilised?
Skilled consultants can play pivotal roles in supporting clinical governance in healthcare organisations by bringing expertise, insights, and objectivity to the table. Their involvement can support leaders to drive a culture of safety and accountability.
Their primary function usually involves identifying gaps and challenges in existing clinical governance systems, proposing effective solutions to enhance the quality of care (such as engaging patients and clinicians), and recommending how these are monitored by the board / principals. They also guide healthcare institutions in setting up robust clinical governance frameworks aligned with the organisation’s goals and regulatory standards.
Consultants may lead audits and assessments to ensure adherence to clinical guidelines and protocols, and assist in interpreting key performance indicators and other data to benchmark performance and identify areas for improvement. They also advise on risk management strategies to mitigate potential threats to patient safety and care quality.
Case study: Larter Consulting supporting Bendigo Community Health Service (BCHS)
Larter was commissioned to review BCHS’ medical services in 2023, including clinical governance. We created a new clinical governance framework and reporting structure for the organisation. This included recommending a Lead Clinician position to oversee clinical governance on an ongoing basis.
The framework helped to address gaps in the structures, roles, and reporting lines related to clinical governance. We recommended the establishment of a dedicated board clinical governance subcommittee (or the evolution of the existing Quality, Safety and Community Experience Committee) to adequately cover clinical governance. We also suggested recruiting an adequately skilled clinician onto the Board and implementing site meetings to identify and table emerging operational and clinical issues or risks.
These recommendations have been actioned by BCHS.
How is your clinical governance system performing?
Clinical governance is a strategic framework that prioritises patient safety, quality of care, and holds healthcare organisations accountable. This approach can transform traditional methods of operation through continuous evaluation and improvement implementation.
Contact us today to discuss your needs to audit or enhance clinical governance.
